Untangle the Healthcare Data Mess
 Untangle the Healthcare Data Mess
Untangle the Healthcare Data Mess
Every Christmas morning we had this unspoken contest of who could wake up with the best morning hair. It gave us all a huge laugh, in fact you had some sort of family pride when you won. Everyone had some sort of tangle mess on top, but my daughter always screamed the loudest when we tried to untangle her mess. Much like our morning hair, in a Health Information Management Department, you will be pleasantly surprised to see how many tangled EMR (Electronic Medical Records) systems and patient records they are sorting through. Icons after icons, in and out of different systems. Your job as an employee of the department will require you to spend an enormous amount of time searching these legacy EMR’s to obtain all the information related to a single patient so that you can fulfill a request from a patient, physician, or attorney. The biggest challenge facing you is there’s no unique identifier that ties all these records together. One might think that there is some coordinated set of standards among healthcare providers. There is not a well-defined way of handling this. Can you require a Medical Records clerk to determine if a “Tony Smith” in one EMR is the same as “Anthony Smith” in another? Does the birth date for Anthony of August 11, 1981, automatically match with 08/12/1981 in the other EMR? Is it the same patient or not? Did someone mistype the wrong day or is there two different people born this close together? This puts the burden of inaccurate decision making on the clerk. Determining if the patient receives a diagnosis or misleads physicians can depend on whether these records are merged or not. Bless those Medical Records clerks because I don’t envy that position.
One Problem
 There has not been a defined universal standard for identifying a patient among physicians practices or healthcare organizations throughout the country. Usually, through these massive implementations of a single EMR, it is enabling a unique identifier for patients called an EMPI (Enterprise Master Patient Index). When healthcare organizations go through these massive EMR migrations or through acquisitions of clinics/physician practices, it is leaving behind the legacy EMR that contains patients records. It is increasing the complexity of patient information that is not uniquely tied together.
There has not been a defined universal standard for identifying a patient among physicians practices or healthcare organizations throughout the country. Usually, through these massive implementations of a single EMR, it is enabling a unique identifier for patients called an EMPI (Enterprise Master Patient Index). When healthcare organizations go through these massive EMR migrations or through acquisitions of clinics/physician practices, it is leaving behind the legacy EMR that contains patients records. It is increasing the complexity of patient information that is not uniquely tied together.
These disparate EMR systems usually just sit out there in a dormant or read-only state to be dealt with at some future time. Not only is it creating complexity in access to patient information, there is a great expense burden carried by keeping these systems up and running. The unique skill set in IT staff, annual maintenance costs to software vendors, and capital costs to keep those systems from reaching their end-of-life. Healthcare organizations have retention policies and state/federal regulations which make it difficult to shut down these systems.
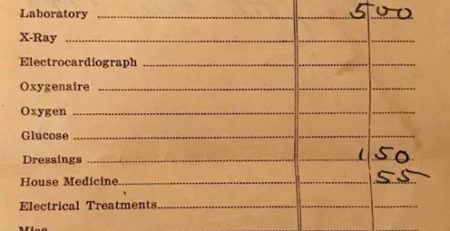
This valuable data in these systems can unlock critical patterns to help the chronically ill, provide a diagnosis to a suffering patient, or improve the quality of care. We are sitting on a gold mine of data that only providers of long ago could only imagine.
The founder of modern nursing and statistician, Florence Nightingale, in 1863 wrote:
“I am fain to sum up with an urgent appeal for adopting…some uniform system of publishing the statistical records of hospitals. There is a growing conviction that in all hospitals, even in those which are best conducted, there is a great and unnecessary waste of life….In attempting to arrive at the truth, I have applied everywhere for information, but in scarcely an instance have I been able to obtain hospital records fit for any purposes of comparison….If wisely used, these improved statistics would tell us more of the relative value of particular operations and modes of treatment than we have means of ascertaining at present.”
Florence Nightingale 1863
4 Major Steps to Take

Step 1 – Application Portfolio
Obtain your application portfolio, which is an inventory of all your systems. This will unlock an enormous amount of information you will need for your business case and legacy systems rationalization efforts. This portfolio should capture not only the name of the application, but you will need things like the contract end date, annual fees, type of data (financial, clinical, etc), current software version, end-of-life version, locations its accessed, servers, database, etc. You will become reliant on a single source of truth and will need to put controls in place to make sure changes are managed accurately.
Step 2 – Design and Plan
This is probably the largest effort and requires good documentation and discussion among key stakeholders. It requires detailed oriented skills that can organize information and documents very well. Some things to consider in this effort:
Scope – You need to know exactly what systems are in scope of rationalizing and the type of data in those systems to accurately put a technical design and plan together. There are 5 buckets I group applications into and its based on the type of data in those applications:
Bucket 1: Clinical, Scheduling systems
Bucket 2: Documents (Scanned Images) Systems
Bucket 3: Financial (Billing) Systems
Bucket 4: Imaging (PACS/CV PACS)
Bucket 5: ERP (HR, Finance, Supply Chain)
Creating several views of your portfolio will assist in your planning and cost efforts. You will know when you will begin to see savings, improve HIM operations, and gain access to a full medical record. You will begin to contain your data to analyze and make improvements to care and operations.
Contract Inventory – Working with legal to gathering up all your contracts is necessary to ensure everything is being handled correctly. It will provide insights into your requirements for termination and breach. Legal input for interpretation of agreements will be necessary, especially when vendors know they are losing your business and their performance drops leaving you in a bind. Avoiding unnecessary costs and additional annual fees because you know when agreements and termination notifications need to go out.
Archive solution design – It is important that the organizations define the requirements for a final resting place or archive of the data. There are critical solution design pieces that need to be considered as it does impact workflow, here is just a couple of example:
-
Will the legacy data need to be accessed through the current EMR or just a look-up in the archive solution?
-
Will AR be worked down prior to migration or will the archive need to be “active” one that continues to capture notes, payments etc?
Total Cost – It is important that you develop out the total cost of the work effort and establish when you will see the benefits of the savings. In a Total Cost model, I like to capture the Capital, One-Time Operating, and On-Going Operational costs. This is critical in building out a business case and your finance folks will have clear visibility into the efforts.
Governance – Are stakeholders that have a vested interest in making decisions that affect their scope of responsibilities. Without governance over what happens to the data, organizations are leaving decision up to those that don’t have a vested interest, like IT. If ownership of data hasn’t been defined, this effort will help tease this out. Governing data should consider:
Data Consistency – Data is reliable and consistent
Data Relevance – Data is useful
Data Accuracy – Data is Free from errors
Data Definition – Specific meaning of the data element
Data Accessibility – Data is easily obtainable and legal to access
It was too difficult or near impossible to manage data stored in a paper record. Today, it can be as we improve our precision in operations and care delivery. Technology has introduced new types of work for organizations that haven’t been there before, governing data is one of them.
EMPI – A well thought out EMPI (Enterprise Master Patient Index or Identifier) will tie patient records together and bring about the necessary outcomes of an organization. As data is migrated and patient records merged decisions to the accuracy and quality of this effort will need to be determined. It will require registration and HIM departments to work more closely together to reduce duplication of records and ensure ongoing accuracy of patients identification. If this is not done well, patient documentation may be on two or more records, creating a patient safety and legal medical record problem.
After the culmination of this work, a well laid out plan and schedule can be established. Resources can be brought together in work teams and execution can occur.
Step 3 – Car Wash Approach
The actual implementation, I like to call the car wash approach. Each application will go through the repeatable process from migration to decommissioning. The phases below do have outlined roles and activities through each phase of the effort. It takes careful management and decision making throughout each phase is critical as you may be running multiple applications at a time through a given phase. A well-organized project manager is important.
Prep Review Extract Translate Load QA Decommissioning Harvest
Step 4 – On-Going
This process can be done much simpler on-going and should be apart of any acquisition or single EMR implementation. It is repeatable and the framework can be used quickly. It will bring new operational relationship and roles going forward around data.
Just like untangling the Christmas morning hair at my house, it can be difficult, but must be done. Healthcare data and the complex number of EMR’s, is Christmas morning. Untangling the mess will make a huge difference to providers of care and most importantly the patient. Having high levels of confidence in your data will make vast improvements to decision making and avoid errors. In LEAN Six Sigma, your statistical analysis efforts are to gain optimal or perfect practice of a process by reducing waste and errors. Untangling the data mess can be very complex yet worth the effort, however, your confidence in your data and records are now much greater that you can really begin to unleash your data strategies.
More articles like this: https://dewingit.net/blog
Services: https//www.dewingit.net/services
Email us: jewing@dewingit.net




Leave a Reply